
A recent medical innovation, the titanium rotary heart developed by BiVACOR, successfully sustained a patient awaiting a heart transplant for eight days, representing a major advancement in artificial heart technology that may soon be approved for long-term use.
Approximately five percent of adults listed for a heart transplant in the US annually do not survive the wait. This patient, however, participated in an FDA Early Feasibility Study at the Texas Heart Institute, receiving BiVACOR’s total artificial heart (TAH), which is designed unlike traditional artificial hearts. The patient managed to survive the critical period until a donor heart was found.
Key Features of the BiVACOR TAH
The TAH employs cutting-edge maglev technology, similar to systems used in high-speed trains, to replace both ventricles of the heart with a single magnetically levitated rotor. This design is not only more durable but also more energy-efficient compared to older models, which rely on diaphragms, membranes, and valves that mimic the natural heartbeat.
For eight days, the patient’s blood was circulated by a device that whirled rather than beat.
Dr. Joseph Rogers, President and CEO of the Texas Heart Institute and the National Principal Investigator of the research, expressed satisfaction with the TAH’s performance, which met their expectations during this first-in-human implantation. The patient’s subsequent recovery was promising, illustrating the potential of the BiVACOR TAH in transforming heart failure treatment.
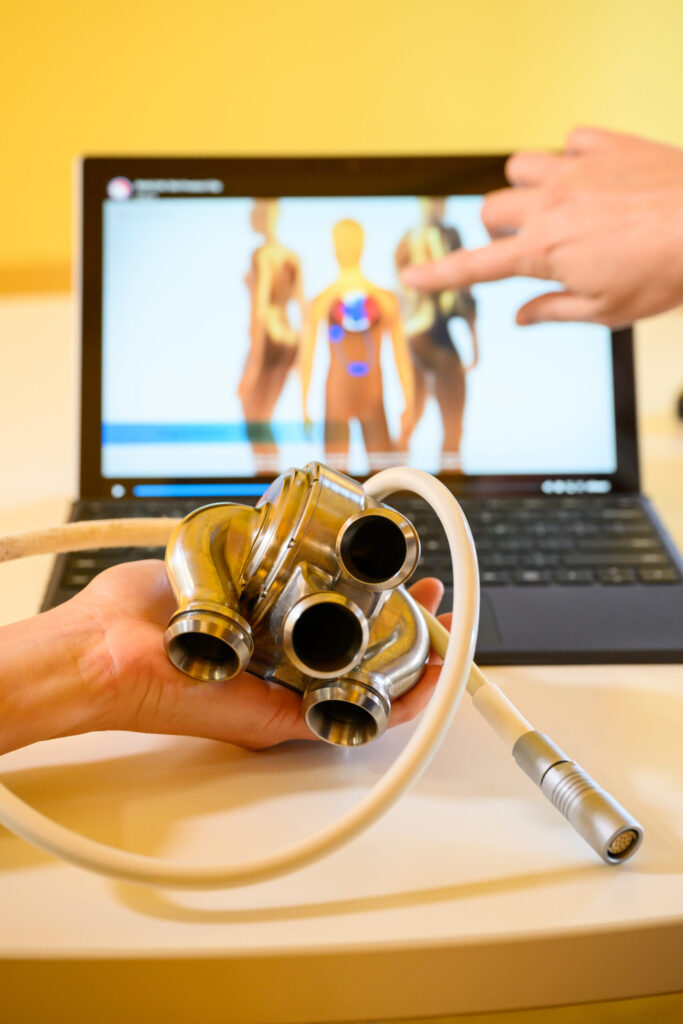
BiVACOR’s device, made from titanium, offers several advantages over earlier artificial hearts. It is designed to be more blood-friendly and maintains inherently balanced blood flows, crucial for preventing complications.
Earlier devices, which typically last only 12 to 18 months due to mechanical wear from approximately 52 million beats per year, are outperformed by the TAH’s durability and lower energy consumption.
The implications of this advancement are significant, given the global impact of heart failure, which affects at least 26 million people, including 6.2 million adults in the US alone.
Despite the high demand, heart transplants are limited, with fewer than 6,000 procedures performed globally each year. The National Institutes of Health in the US estimates that up to 100,000 patients could benefit immediately from a ventricular assist device (VAD) or a TAH like BiVACOR’s.
Future Prospects for the BiVACOR TAH
Looking forward, Dr. Alexis Shafii, Surgical Director of Heart Transplantation at Baylor St. Luke’s Medical Center and Associate Professor of Surgery, Cardiothoracic Transplant & Circulatory Support at Baylor College of Medicine, anticipates that the BiVACOR TAH could save many lives and significantly improve the quality of life for patients lacking alternative therapies.
With the first implantation deemed a success, BiVACOR plans to enroll four additional patients in the study, moving closer to potential FDA approval for long-term use of the device.
Featured Image courtesy of BiVACOR
Follow us for more healthcare and technology updates.
